
What to Know About Borderpolar

One-on-One Counseling in Arizona for Life's Challenges
Every day is a chance to start over. Our trauma-informed therapists will meet you where you are — in person or online — so you can process your experiences and become the person you want to be.
You may have heard the term borderpolar on social media or in conversation. While borderpolar is a term, not a diagnosis, it does encapsulate something curious that clinicians have been seeing for years in therapy and that many people live with day to day.
The term borderpolar comes from the combination of two comorbid diagnoses: borderline personality disorder (BPD) and bipolar disorder. People who identify with this term often experience overlapping traits from both conditions, and this overlap can make assessments, treatments, and even self-understanding much more difficult.
To understand what borderpolar really means, let’s clarify the differences between BPD and Bipolar Disorder, explore how the two can overlap in real life, and identify the steps you can take if you or someone you care about is navigating these challenges.
Borderline Personality Disorder vs. Bipolar Disorder
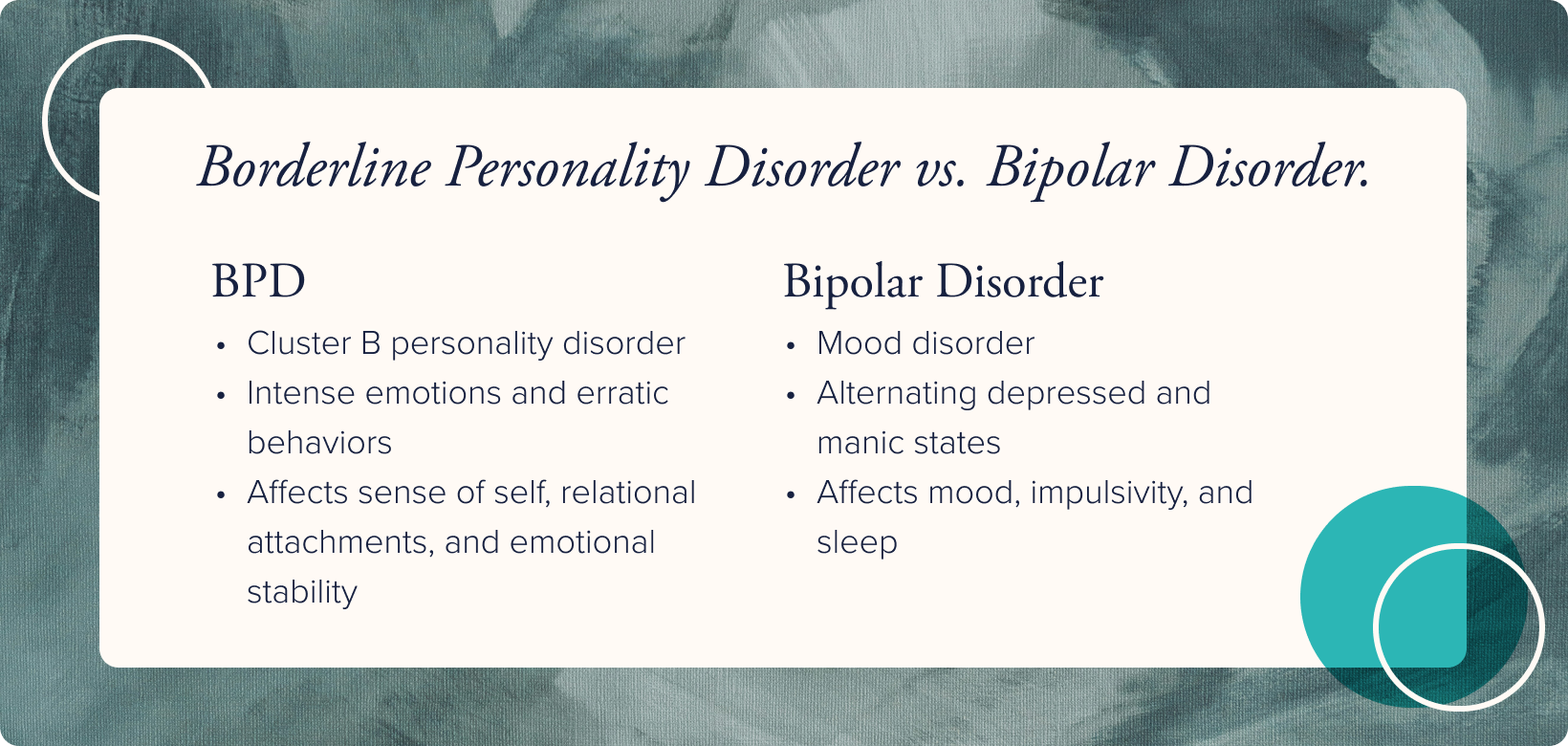
BPD and bipolar disorder are separate conditions that belong to entirely different diagnostic categories:
BPD is classified as a cluster B personality disorder, which is a group marked by intense emotions and erratic behaviors. This condition can profoundly affect an individual’s sense of self, relational attachments, and emotional stability.
Bipolar disorder is a type of mood disorder that can be broken down into three distinct diagnoses: bipolar I, bipolar II, and cyclothymic disorder. Bipolar can be seen in family systems, impacts mood, impulsivity, and sleep, and is characterized by shifts from depressed to manic states.
Similarities Between BPD and Bipolar Disorder
Although BPD and bipolar disorder are two distinct disorder, they share many of the same symptoms. This overlap is partially responsible for the term borderpolar, as it describes someone that experiences the symptoms and challenges from both conditions.
Some of the symptoms that BPD and bipolar disorder have in common include:
- Sudden and intense mood changes
- Impulsive or risky behaviors
- Strong emotions that are difficult to regulate
- Interpersonal difficulties
- Self-esteem issues
- Challenges in daily functioning
These shared symptoms are part of what makes the two conditions easy to confuse for one another. To add to this confusion, these conditions are often comorbid, meaning it’s common for someone with one condition to also have the other.
Read our related guide for more information on bipolar disorder, its symptoms, and how it’s treated.
5 Things You Should Know About Borderpolar
Navigating the overlap between borderline personality disorder (BPD) and bipolar disorder can feel overwhelming and even confusing at times. To help make sense of it, let’s go over five essential things to know for anyone affected by or supporting someone with borderpolar symptoms.
Receiving an Accurate Diagnosis for BPD and Bipolar Disorder
It can take a long time for someone to receive a correct diagnosis for both BPD and bipolar disorder. The symptoms of BPD can make it difficult to identify other co-morbid diagnoses, and bipolar disorder are notoriously difficult to diagnose. In fact, it can even take several years before someone receives an accurate diagnosis for a bipolar disorder.
On their own, each disorder is complex and requires thorough assessments to accurately diagnose. When they occur together, it can be even more challenging to untangle each condition, and this further delays someone from getting the appropriate treatment and support they need.
Treating BPD and Bipolar Disorder
There are no distinct medications specifically for BPD, but many psychopharmacological medications treat bipolar disorder. Medication and therapy are most often needed for managing bipolar disorder, while specific therapy modalities effectively treat BPD.
BPD was previously thought to develop through unhealthy attachments and trauma in childhood. Recent research indicates that BPD also has a genetic component, as does bipolar disorder.
Stigmas Surrounding BPD and Bipolar Disorder
Even in the clinical mental health communities, BPD carries a stigma of being difficult to treat. This often comes from the difficulties that a person struggling with BPD has in their interpersonal relationships, sense of self, and management of emotions.
Thankfully, as research focuses more on finding the cause and evolution of BPD, more understanding and compassion are growing for struggling individuals.
A bipolar diagnosis often has its own stigmas due to the need for medications, the swings in mood that impact functioning, and the occurrence of hallucinations and delusions present in several more severe cases. Bipolar disorder with psychotic features may be confused with schizophrenia outside of clinical treatment and make an individual afraid to seek help and support.
Impacts of Living With BPD and Bipolar Disorder
Both BPD and bipolar disorder are serious diagnoses and require treatment for a person to be healthy and well. Those suffering from symptoms of BPD may fear abandonment and have complicated and short-lived relationships, and they may also abuse substances and self-harm to self-soothe or cope.
Those who struggle with bipolar disorder symptoms may have periods of high energy, lack of sleep, changes in the sense of self, and impulsivity for a time and then sink into depression, low energy, and an increased need for sleep.
These diagnoses cause symptoms that may make it challenging to be a consistent partner, employee, and friend. There are some overlaps in symptoms that may look like connection seeking, loneliness, and feelings of not being normal. When they occur together, they may cause the individual heightened distress, emotional instability, and feelings of helplessness.

Hope for Those Living With BPD and Bipolar Disorder
Over time, living with an incorrect or delayed diagnosis can erode hope. For someone with BPD or bipolar disorder who is misdiagnosed or untreated, quality of life may be significantly impacted. Intense feelings of helplessness and being a “victim of circumstance” are common, as the person may not recognize their experiences as symptoms of a mental health disorder and instead blame themselves. This can be especially difficult for those who already feel marginalized due to the effects of their struggles on daily functioning and relationships.
Although both diagnoses are serious and require targeted treatment, there is significant hope for those with BPD or bipolar disorder.
With the right therapist, doctor, and treatment plan, someone experiencing borderpolar symptoms can lead a healthy, fulfilling life. Once proper support is in place, many individuals regain stability, manage daily challenges, and even thrive.
Find the Support You Deserve at Inner Balance
If you or someone you know displays symptoms of BPD or bipolar disorder, know that there is help available. Reaching out for support isn’t a moral failing, it’s a courageous step towards understanding, healing, and growth.
At Inner Balance, we’ll work with you on an individual level to come up with a treatment plan that’s personalized to you and your mental health journey. Whether you’re suffering from BPD, bipolar disorder, or both, we can help you get the diagnoses and treatments you need to live the life you deserve.
Reach out today to connect with a mental health professional and learn how to live life on your terms.
Related blog articles
Sign up for our newsletter
Sign up with your email address to receive news and updates.
Get started
Request a consultation

-03%201.png)




