
Depression
A battle for mental security

One-on-One Counseling in Arizona for Life's Challenges
Every day is a chance to start over. Our trauma-informed therapists will meet you where you are — in person or online — so you can process your experiences and become the person you want to be.
Depression is one of the most common mental illnesses worldwide. According to recent data from the National Institute of Mental Health (NIMH), 21.0 million adults (18+) and 4.1 million adolescents (12-17) report having one or more depressive episodes.
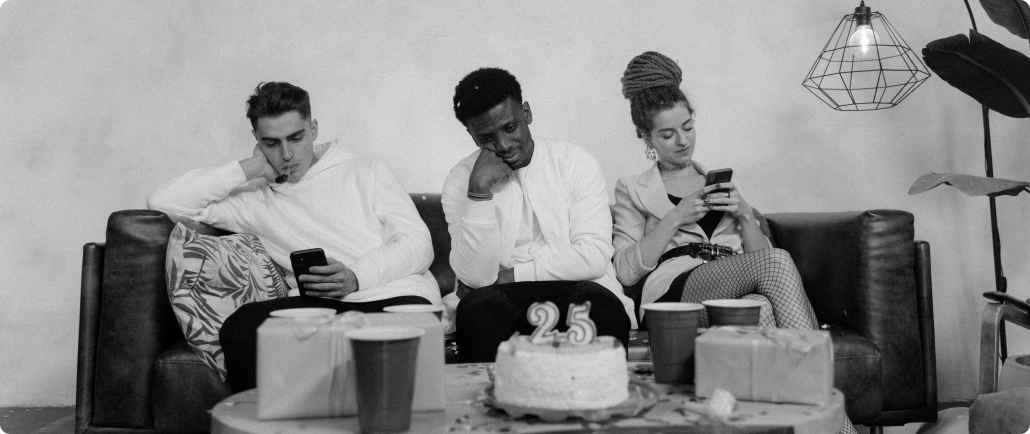
Depression is more than feeling down. This condition may convince you that you’re alone, inadequate, or powerless, causing things that once brought you joy to leave you feeling empty. Depression is a master storyteller and deceiver.
It makes little difference how intelligent, successful, or well-liked you are—depression can leave you feeling cornered and exhausted.
What is Depression?
According to the American Psychiatric Association, depression is a common and serious medical illness that affects how a person thinks, feels, and behaves. There is no “on/off” switch for depression. As artist Anthony Benevidez expressed it:
“Depression is living in a body that fights to survive, with a mind that tries to die.”
Depression can lead to emotional, social, and physical problems—which decrease a person’s ability to function day-to-day. It can even cause a person to question their role, abilities, and purpose.
What are the Symptoms of Depression?
Symptoms can vary depending on depression type. Below is a list of common symptoms linked to depression:
- Body aches, headaches, cramps, or digestive problems that do not ease with treatment
- Changes in appetite or unplanned weight changes (gain or loss)
- Decreased energy or oversleeping
- Difficulty concentrating, remembering, or decision-making
- Insomnia, early morning awakening, or fatigue
- Loss of interest or pleasure in activities
- Persistent feelings of sadness, anxiety, or emptiness
- Constant feelings of irritability, frustration, or restlessness
- Incessant feelings of guilt, worthlessness, or helplessness
- Suicidal ideation or intentional self-harm
Those experiencing depression will experience a combination of symptoms most of the day, nearly every day, for two weeks or longer.
Is Depression the Same as Grief?
Grief is a common and normal response to loss. Most people grieve following the death of a loved one, relationship separation, or job loss. These people often claim to feel depressed.
There is sometimes a misperception that grief and depression are the same. Both grief and depression involve intense sadness and withdrawal but differ in other ways.
Some of these include:
- Duration: In grief, painful feelings come in waves; with depression, painful feelings remain for two weeks or longer.
- Self-esteem: In grief, a person maintains high self-esteem; in depression, feelings of worthlessness or self-loathing are common.
- Thoughts of death: In grief, thoughts of death may surface if fantasizing about joining a deceased loved one. In depression, thoughts of death are due to feeling worthless, undeserving, or burdensome to others.
Anyone can experience loss and grief, however, not everyone will experience clinical depression because of grief.

What Causes Depression?
Millions of chemical reactions make up the system responsible for moods, perceptions, and life experiences. Researchers used to believe that depression was caused by an over or underabundance of specific brain chemicals (neurotransmitters). We now know that this isn’t entirely true.
Depression does involve neurotransmitters, but it is not a simple matter of one chemical being too low or too high. Research by Harvard Medical School suggests that many chemicals are involved, working inside and outside the nerve cells to affect the body.
Depression is a complex illness because there is no one specific cause for it. There are several factors that contribute to depression, including genetics, stress, and problems with mood regulation in the brain.
Does Anything Increase the Risk of Depression?
According to the Depression and Bipolar Support Alliance (DBSA), certain factors increase a person’s risk of developing clinical depression. These include:
- Age: Older adults are at a higher risk of depression, worsened by living alone and lack of social support.
- Gender: Women are twice as likely as men to experience clinical depression. Hormonal changes may play a role.
- Genetics: A family history of depression increases its risk of appearing in later generations.
- Major Events: Depression is more than the body’s natural response to stressful life events or loss. Grief can increase a person’s risk of depression, but so can a move, marriage, or graduation.
- Medications: Some prescription medications can increase a person’s risk of depression.
- Serious Illness: Other medical conditions or illnesses can sometimes trigger depression.
- Substance Misuse: About 20% of people suffering from substance misuse also experience clinical depression. Drugs and alcohol tend to aggravate aggression long-term, even if providing temporary relief.
- Trauma: There is a link between physical, sexual, and emotional trauma and depression later in life.
How Many Types of Depression are There?
There are a variety of criteria medical professionals use to differentiate unique depression types. Some have obvious causes, while others may seem to appear out of nowhere.
Here is a list of depressive disorders in the diagnostic classification of the DSM-5.
- Bipolar depression: Formerly called manic depression or manic-depressive illness, bipolar disorder causes people to go through extreme low- and high-energy periods. In the high-energy (manic) periods, people tend to feel “up” in happy or irritable ways. The low-energy (depressive) periods cause people to feel “down” in sad or hopeless ways.
- Disruptive mood dysregulation disorder (DMDD) is a childhood condition with frequent and intense temper outbursts. The child will show extreme irritability, anger, and social impairment. Diagnosis for a child between the ages of 6-17 requires symptoms to be present on an almost daily basis for a year or longer.
- Major depressive disorder (MDD) is a condition characterized by persistent sadness and lack of interest in life or activities. Diagnosis requires overwhelming symptoms that last longer than 2 weeks and episodes separated by at least 2 months.
- Perinatal/Postpartum Depression can occur during pregnancy or up to a year after the birth or adoption of a child. People with postpartum depression may experience frequent crying spells, fatigue, guilt, anxiety, or trouble caring for their child.
- Persistent depressive disorder (PDD): Also known as dysthymia, symptoms of PDD are similar to MDD but less severe. To be diagnosed with PDD, people must experience symptoms for two years or longer.
- Premenstrual dysphoric disorder (PMDD) is a severe form of premenstrual disorder (PMS). People with PMDD might have PMS symptoms in addition to severe anxiety, extreme irritability, mood changes, depression, or suicidal thoughts. PMDD affects people in the days or weeks leading up to their menstrual period.
- Psychotic depression: People with psychotic depression have severe depressive symptoms combined with delusions/hallucinations. They may have opinions that are not based on reality or see, hear, and feel things that aren’t there.
- Seasonal affective disorder (SAD): Commonly referred to as seasonal depression, SAD is triggered by the changing seasons. This type of depression usually starts in the fall/winter and goes away in the spring/summer. Common symptoms include lingering sadness, anxiety, carbohydrate cravings, weight gain or loss, extreme fatigue, and lack of energy.
I think I’m Depressed. What Do I Do?
Don’t worry—you’re not alone, and help is available.
Depression has a high treatment success rate, even in acute cases. The earlier depression treatment begins, the more effective it is.
Having Suicidal Thoughts?
If you or someone you know is currently feeling suicidal, immediately call the 24/7 Suicide & Crisis Lifeline at 988.
This Lifeline provides support for people in duress and shares resources for prevention and crisis.
Get started
Request a consultation

More Resources
Apathy

Postpartum Depression

Parentification
Here’s how it works
We know asking for help is hard, that’s why we want to make it easy for you.
Reach out
Show up
Feel better
Sign up for our newsletter
Sign up with your email address to receive news and updates.
-03%201.png)
